Healthcare organizations today rely on an average of 18 different health information systems, yet 89% of hospitals still identify data fragmentation as their biggest challenge. When patient records are scattered across disconnected platforms, providers face incomplete medical histories that directly impact care quality, diagnostic accuracy, and treatment outcomes.
This is not just an IT issue, it is a critical patient care concern. Without a unified view, even the most skilled clinicians may struggle to deliver safe, timely, and personalized care. Healthcare data integration bridges this gap by consolidating fragmented information into a single, comprehensive patient record. Through medical data integration, hospitals can align lab results, imaging data, prescriptions, and clinical notes into one accessible source of truth.
The adoption of data integration in healthcare is transforming operations across the industry. From enabling real-time healthcare data integration that supports emergency decisions to leveraging clinical data integration for chronic disease management, the benefits are measurable. Modern healthcare data integration platforms built on interoperable standards ensure compliance, enhance collaboration, and improve patient safety.
As the healthcare data integration market continues to expand, organizations that embrace scalable, standards-driven solutions will be best positioned to improve outcomes, streamline operations, and build trust through secure, patient-centered care.
What is Healthcare Data Integration?
Healthcare data integration is the structured process of unifying patient information from multiple, often siloed, systems into a single, accessible format. Unlike basic data collection, it standardizes, cleanses, and organizes medical records, lab results, imaging scans, and administrative details into a coherent patient profile through effective data integration techniques.
This process spans EHRs, laboratory systems, pharmacy platforms, imaging repositories, and even patient-generated data from IoT devices and wearables. By enabling interoperability through healthcare data integration standards, providers gain a holistic view of patient histories, conditions, and treatment responses.
With the healthcare industry generating over 2.3 exabytes of data daily, fragmented access hinders clinical decision-making. Clinical data integration closes this gap, empowering healthcare providers with real-time insights that enhance diagnoses, optimize treatment plans, reduce errors, and ultimately improve patient safety and outcomes.
Why Data Integration Is Crucial in Healthcare?
The digital transformation of healthcare was meant to simplify data management, yet it has unintentionally created silos. Each department, specialty, or facility often runs its own system, leaving vital patient data scattered across disconnected platforms. This lack of healthcare data integration impacts not only efficiency but also care quality and patient safety, underscoring the close link between data analytics and digital transformation in modern healthcare.
By using advanced healthcare data integration platforms and adopting consistent standards, providers can break silos, cut costs, and build a connected ecosystem for patient-centered care.
Clinical Impact of Disconnected Systems
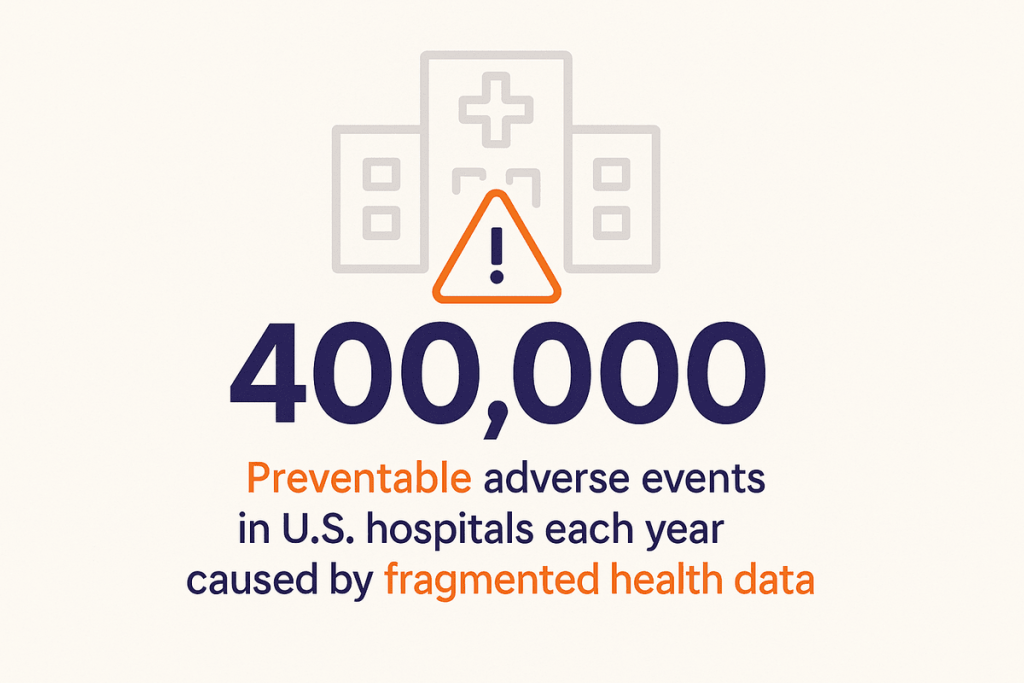
Incomplete access to medical histories exposes providers to serious risks. Missing details on allergies, prior treatments, or prescriptions can result in repeat tests, delayed diagnoses, or even harmful decisions.
Research shows fragmented health data contributes to nearly 400,000 preventable adverse events in U.S. hospitals each year, underscoring the urgent need for medical data integration and clinical data integration to support safer, more accurate care.
Financial and Operational Costs
Data silos carry a heavy financial burden. U.S. healthcare organizations spend over $30 billion annually on duplicate tests and imaging because one system’s results remain invisible to another.
Administrative teams also waste hours reconciling conflicting records or re-entering duplicate data time and resources that should be directed toward patient care.
Population Health and Quality Measurement
Without strong health data integration, organizations struggle to monitor chronic conditions, measure care quality, or track population health outcomes. These gaps weaken value-based care initiatives, where reimbursement depends on demonstrating measurable improvements in outcomes and cost efficiency through comprehensive business intelligence in healthcare.
Key Benefits of Data Integration in Healthcare
Healthcare data integration has become a business-critical strategy for modern organizations. By breaking down silos and unifying data across disparate systems, providers not only improve clinical outcomes but also reduce costs, strengthen compliance, and gain the agility required to succeed in a rapidly evolving healthcare landscape.
Implementing a clear data integration strategy ensures these efforts remain scalable and aligned with organizational goals.
With the right healthcare data integration platform, organizations can experience these following benefits that fuel both patient-centered care and long-term business growth:
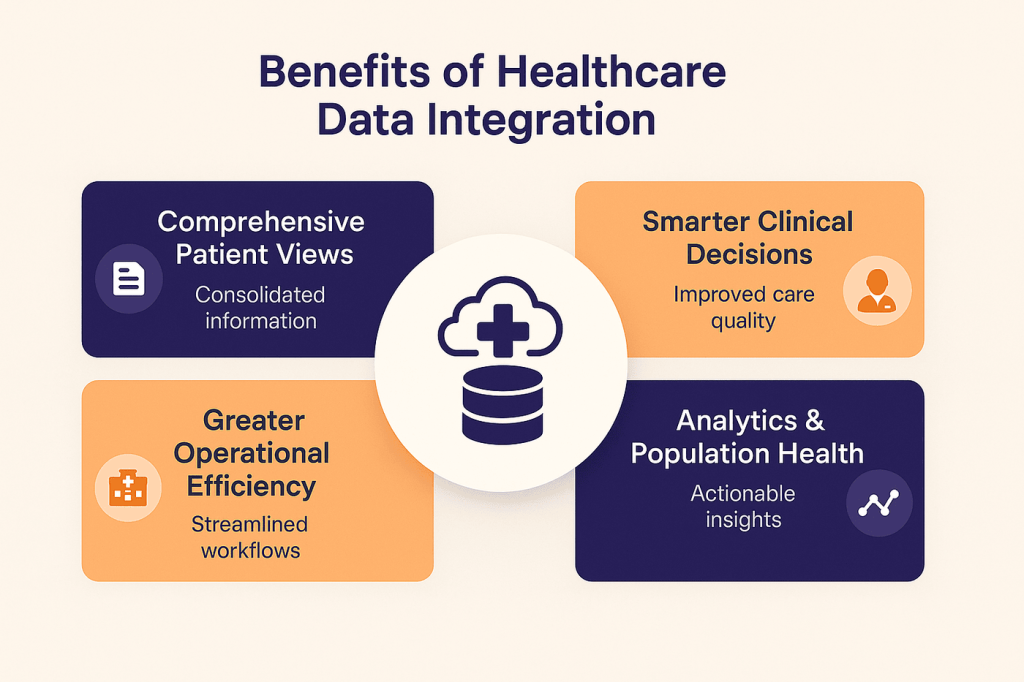
1. Comprehensive Patient Views
Through medical data integration, clinicians gain a complete, 360-degree view of patient timelines including lab results, imaging, medications, and provider notes. This holistic perspective reduces diagnostic errors and accelerates treatment decisions.
2. Smarter Clinical Decision-Making
With clinical data integration, decision support systems become significantly more effective. Providers gain access to complete patient records, enabling real-time analytics in healthcare, drug interaction alerts, and evidence-based recommendations. Geisinger Health’s integration of genomic and medical data improved cancer treatment outcomes by 31%, showcasing the power of precision medicine fueled by integrated datasets.
3. Operational Efficiency Gains
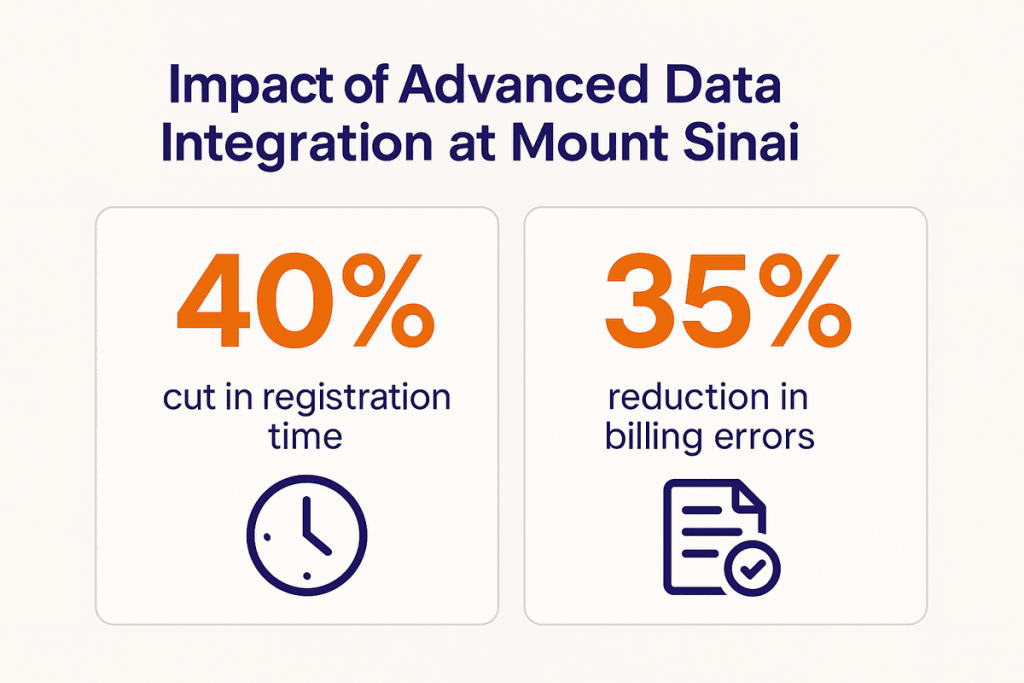
Beyond clinical benefits, healthcare data integration standards streamline workflows and reduce manual processes. Mount Sinai Health System achieved a 40% faster registration process and 35% fewer billing errors after implementing an advanced integration platform allowing staff to focus on patient care and revenue optimization through data engineering in healthcare.
4. Foundation for Analytics & Population Health
Integrated data also lays the foundation for advanced healthcare analytics and predictive modeling. Kaiser Permanente’s use of real-time healthcare data integration reduced 30-day readmission rates by 18%, improving both outcomes and cost efficiency while maximizing the benefits of data analytics in healthcare.
At Folio3, our healthcare data analytics consulting services help organizations achieve these kinds of measurable results. By enabling interoperability, breaking silos, and building scalable, compliant infrastructures, we ensure your data delivers maximum value for patients and your business alike.
For instance, Folio3 partnered with Phamily, a digital health innovator, to transform fragmented systems into a unified, HIPAA-compliant, and analytics-ready data ecosystem. This collaboration enabled smooth EHR integration, real-time reporting, and scalable patient-centric care.
Challenges of Data Integration in Healthcare
Despite its benefits, healthcare data integration comes with several challenges that organizations must overcome. So, healthcare organizations face several significant challenges when implementing data integration initiatives. Understanding these obstacles helps organizations prepare more effective implementation strategies:
- Lack of Standardization & Interoperability: Different EHRs, lab systems, and pharmacy platforms use varying data formats and coding standards, making seamless medical data integration difficult without middleware or universal protocols.
- Data Quality & Consistency: Duplicate records, incomplete profiles, and outdated information can undermine clinical data integration efforts, reducing accuracy and trust in patient data.
- Privacy & Security Risks: Centralized platforms increase vulnerabilities. Maintaining HIPAA compliance, securing health data integration pipelines through healthcare data security measures, and ensuring robust access controls are critical to protecting patient information.
- High Implementation & Maintenance Costs: Building a scalable infrastructure for healthcare data integration requires substantial investments in infrastructure, licenses, and ongoing maintenance, which can strain budgets, especially for smaller providers.
- Organizational & Cultural Barriers: Resistance to workflow changes and fears of automation can slow adoption. Success depends on effective change management and demonstrating clear value for both clinicians and administrators.
Partner with Folio3 to overcome cultural barriers and drive seamless adoption with proven change-management strategies.
Proven Practices for Healthcare Data Integration
Successful healthcare data integration projects follow common patterns that maximize benefits while minimizing implementation risks. These proven practices address both technical and organizational aspects of integration initiatives.
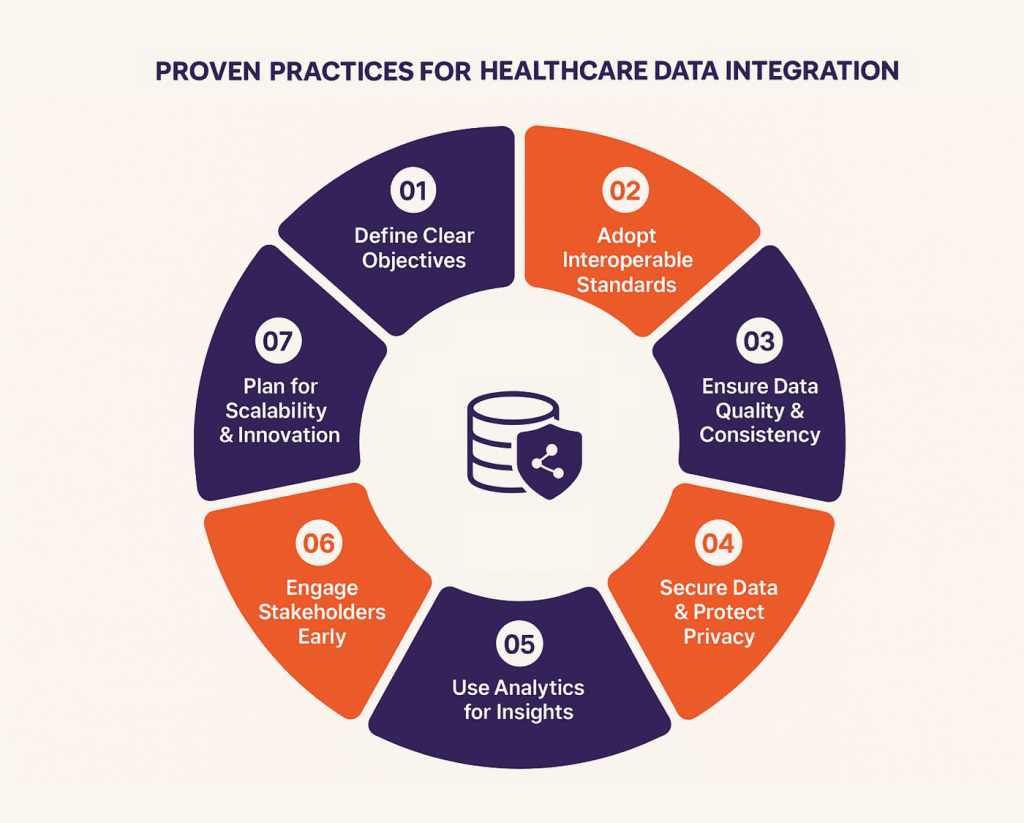
1. Define Clear Objectives
Successful healthcare data integration projects begin with measurable goals, such as reducing duplicate tests, improving medication safety, or enabling population health analytics. Clear objectives guide technology choices, ensure alignment with business priorities, and help measure success across clinical and operational outcomes.
Teams often partner with experts in data engineering services to design these objectives and ensure the integrated environment can handle large-scale, complex datasets efficiently.
2. Adopt Interoperable Standards
Using interoperability standards like HL7 FHIR, DICOM, and IHE simplifies medical data integration and ensures long-term system compatibility. These standardized frameworks reduce custom development, streamline data exchange, and support compliance while creating scalable foundations for enterprise data integration across connected healthcare ecosystems.
3, Ensure Data Quality & Consistency
Without high-quality data, even the best clinical data integration systems fail. Cleansing, validation, and ongoing monitoring through proper data governance strategy eliminate duplicates, fix inconsistencies, and standardize formats, ensuring providers gain accurate, reliable, and actionable insights for improved patient care and decision-making.
4. Secure Data and Protect Privacy
Integrated platforms must safeguard sensitive patient information. Robust healthcare data integration platforms use encryption, access controls, and audit trails to maintain HIPAA compliance. Advanced privacy settings allow secure sharing while protecting patient consent, reducing cyber risks, and maintaining trust.
5. Use Analytics Tools for Insights
Smooth integration creates a strong foundation for healthcare analytics and AI adoption. Unified data enables predictive modeling, population health management, and real-time insights that improve outcomes, optimize resources, and support evidence-based decision-making across the care continuum.
Many organizations enhance these efforts by partnering with experts in data and analytics services to design scalable solutions that turn integrated information into actionable intelligence.
6. Engage Stakeholders Early
Integration success depends on user adoption. Engaging clinicians, administrators, and IT teams early ensures alignment, reduces resistance, and supports workflow optimization. Training, clear communication, and demonstrating value foster smoother transitions to integrated health data systems.
7. Plan for Scalability & Innovation
Future-ready healthcare data integration solutions must evolve with new technologies, data sources, and clinical demands. Cloud data integration platforms offer flexibility, scalability, and reduced infrastructure burdens, enabling organizations to adapt quickly while maintaining security, performance, and compliance.
How Do Different Types of Healthcare Data Create Unique Integration Challenges?
Healthcare data integration takes many forms depending on the source and purpose of data. From clinical systems to insurance records, each type of integration plays a role in creating a complete patient view and supporting operational efficiency. Below is a breakdown of the most common types:
| Type of Integration | Description | Key Benefits | Integration Challenges | Technical Requirements |
| EHR Integration | Combines electronic health records across hospitals, clinics, and care settings. | Complete patient histories, fewer duplicate tests, improved care coordination. | Vendor lock-in, interoperability issues, high data volumes. | HL7/FHIR standards, API connectivity, secure data mapping. |
| Clinical Data Integration | Merges lab results, imaging, and diagnostic reports into unified systems. | Supports accurate diagnoses, enables evidence-based decision-making. | Variations in imaging formats and lab standards, latency in updates. | DICOM support, real-time data pipelines, standardized clinical terminologies. |
| Administrative & Operational | Integrates scheduling, billing, and workflow data. | Reduces manual tasks, decreases errors, improves operational efficiency. | Legacy billing systems, inconsistent data entry practices. | API middleware, RPA (robotic process automation), database normalization. |
| Pharmacy & Medication Data | Connects prescribing systems, pharmacy records, and medication histories. | Prevents drug interactions, improves medication adherence, enhances patient safety. | Drug naming variations, prescription system interoperability, compliance challenges. | NCPDP standards, integration with e-prescription platforms, secure audit trails. |
| Patient-Generated & Wearable | Incorporates data from wearables, apps, and home monitoring devices. | Enables remote monitoring, supports chronic care management, encourages engagement. | Device diversity, inconsistent data quality, patient privacy concerns. | IoT platforms, API-based wearable integration, HIPAA/GDPR-compliant data ingestion. |
| Claims & Insurance Data | Links claims, authorizations, and payer records with clinical data. | Streamlines reimbursements, reduces denials, supports value-based care. | Payer-provider misalignment, slow claims processing, varied coding standards. | EDI standards, payer APIs, automated claims reconciliation tools. |
| Health Information Exchange | Facilitates secure sharing of patient data across different organizations and providers. | Improves care continuity, speeds up emergency care, strengthens collaboration. | Security risks, data governance issues, lack of universal participation. | HIE platforms, blockchain-enabled security, strict identity and access management. |
How to Measure Success & ROI for Healthcare Data Integration?
Measuring the success of healthcare data integration requires a structured approach that captures clinical, operational, and financial outcomes. By aligning metrics with organizational goals, providers can ensure that data integration in healthcare delivers real value.
A well-executed measurement strategy not only proves ROI but also reinforces the importance of data integration in healthcare as a driver of both patient safety and organizational efficiency. Here’s how you can measure success and ROI for healthcare data integration:
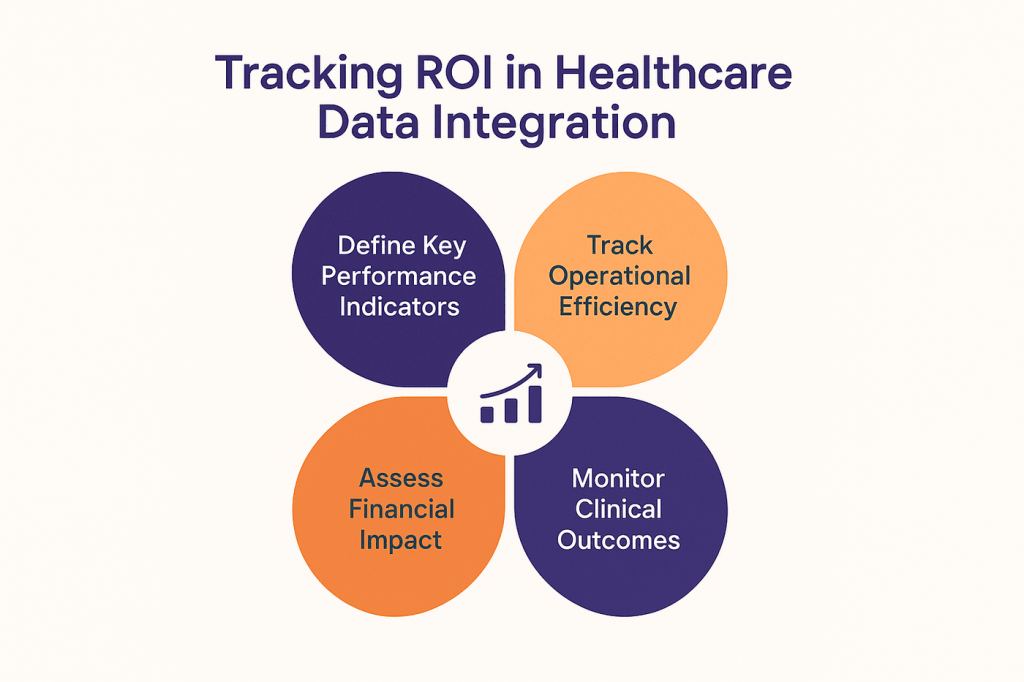
1. Define Key Performance Indicators (KPIs)
Organizations should establish baseline metrics before implementation. Clinical KPIs may include diagnostic accuracy, medication safety, and care coordination, while operational KPIs focus on efficiency, error reduction, and patient satisfaction. A balanced approach ensures that improvements are visible across both clinical and administrative functions.
2. Track Operational Efficiency
Integrated systems streamline workflows by reducing duplicate testing, minimizing manual data entry, and improving billing accuracy. Metrics like registration time, staff productivity, and error rates provide clear indicators of how medical data integration impacts day-to-day operations and supports business intelligence benefits.
3. Assess Financial Impact
Healthcare data integration often translates into measurable financial returns. Cost savings emerge from fewer redundant tests and optimized resource utilization, while improved billing accuracy and reduced claim denials boost revenue. In the long run, better performance in value-based care programs enhances reimbursements.
4. Monitor Clinical Outcomes
Ultimately, the success of clinical data integration lies in improved patient outcomes. By consolidating data, organizations can better track treatment effectiveness, reduce adverse events, and enhance care quality. On a broader scale, health data integration strengthens population health management by identifying trends and enabling proactive interventions through advanced predictive analytics techniques.
Healthcare Data Integration Real-World Examples & Case Studies – What Works in Practice?
Healthcare organizations across different settings have demonstrated that effective data integration can generate significant improvements in patient care and operational efficiency. These following Healthcare Data Integration use cases provide concrete evidence of integration benefits and implementation approaches:
1. Kaiser Permanente’s Comprehensive EHR Integration
Kaiser Permanente created one of healthcare’s most successful integrated data platforms by standardizing on a single EHR system across its entire network of hospitals and clinics. This integration enables clinicians to access complete patient histories regardless of where care was previously provided within the Kaiser system.
Clinicians also use healthcare dashboards to visualize real-time patient metrics, helping reduce duplicate laboratory tests by 40% and shorten emergency department visit times by an average of 25 minutes. Chronic disease management improved significantly, with diabetic patients showing 30% better glucose control when providers could access comprehensive treatment histories and medication adherence data.
2. Mayo Clinic’s Precision Medicine Integration
Mayo Clinic integrated genomic sequencing data with traditional clinical records to support personalized treatment approaches. This integration combines genetic markers, family history, clinical presentation, and treatment response data to guide therapy selection for cancer patients and rare disease cases.
The integrated approach improved treatment response rates by 35% for specific cancer types while reducing adverse reactions from medications that patients couldn’t metabolize effectively based on their genetic profiles. The platform also accelerated clinical research by enabling researchers to identify patient cohorts with specific genetic and clinical characteristics.
3. Mount Sinai’s Population Health Analytics
Mount Sinai Health System integrated patient data across its network to support population health management initiatives. The platform combines clinical data with social determinants of health information through customer data integration approaches to identify patients at high risk for complications or hospital readmissions.
Their predictive analytics identified patients with diabetes who were likely to develop complications, enabling proactive interventions that reduced emergency department visits by 28% and improved medication adherence rates by 45% among high-risk populations.
4. Geisinger’s Predictive Analytics Platform
Geisinger integrated patient records with artificial intelligence tools to develop predictive analytics in healthcare models for early disease detection and intervention. The platform analyzes patterns in laboratory results, vital signs, and clinical notes to identify patients at risk for sepsis, heart failure, and other serious conditions.
The early warning system enabled interventions that reduced sepsis mortality rates by 18% and decreased average length of stay for heart failure patients by 2.1 days. The integration also supported clinical research that led to new treatment protocols adopted by other healthcare organizations.
5. Cerner’s Health Information Exchange Network
Cerner developed integration platforms that enable multiple healthcare organizations to share patient data through health information exchanges. This data integration architecture allows hospitals, clinics, and specialty practices to access patient records even when they use different EHR systems.
The network reduced medication errors by 31% in emergency departments by providing access to complete medication histories from other providers. Patient satisfaction improved due to reduced redundant questioning and faster treatment initiation based on available medical histories.
How Folio3 Drives Healthcare Data Integration Success?
Successfully navigating the complexities of healthcare data integration requires more than just connecting systems—it demands a secure, scalable, and intelligent approach tailored to the realities of modern healthcare. Folio3 empowers healthcare organizations with end-to-end solutions that break down silos, enable interoperability, and unlock the true value of patient data.
1. Smooth EHR Integration
Our expertise ensures smooth integration across diverse EHR platforms, clinical systems, and legacy applications. By consolidating medical records, lab results, and imaging data into a single patient view, we help providers achieve comprehensive clinical data integration that supports better diagnosis and treatment.
2. Secure & Compliant Architecture
With strict adherence to healthcare data integration standards such as HIPAA and GDPR, we design platforms that protect sensitive patient information. Advanced encryption, role-based access, and real-time monitoring ensure security without compromising performance.
3. Real-Time Data Access
Folio3 enables real-time data integration, giving clinicians and administrators immediate access to critical information. This minimizes delays, prevents redundant testing, and improves care coordination across teams and facilities.
4. Advanced Analytics Ready
Our solutions are designed with future-ready capabilities, ensuring integrated data is prepared for predictive analytics, population health management, and business intelligence. This positions organizations to thrive in the growing healthcare data integration market and highlights the value of expert data integration consulting for long-term scalability.
5. Custom Workflows & Automation
Every healthcare provider has unique needs. We build healthcare data integration platforms with configurable workflows and automation, reducing administrative burdens while enhancing operational efficiency.
For organizations leveraging the Snowflake Healthcare Data Cloud, these tailored integrations can seamlessly connect diverse data sources, making it easier to scale analytics and maintain compliance without disrupting daily operations.
Turn fragmented healthcare data into a unified, analytics-ready ecosystem with Folio3’s secure, real-time integration solutions.
Future Trends in Healthcare Data Integration
The future of healthcare data integration is being shaped by emerging technologies and evolving industry standards. These trends are driving innovation in patient care, data security, and operational efficiency.
1. Cloud-Based Solutions and APIs
The shift toward cloud-based platforms and open APIs is redefining data integration in healthcare. Cloud ecosystems make it easier for providers to connect disparate systems, scale on demand, and support advanced applications without the limitations of legacy infrastructure.
2. Artificial Intelligence and Machine Learning
AI and ML are transforming clinical data integration by analyzing large, integrated datasets to deliver predictive insights. From personalized treatment recommendations to early disease detection, these technologies enhance both patient care and resource utilization while enabling generative AI implementation in healthcare workflows.
When paired with AI data extraction, they can automatically pull key information from diverse sources, ensuring that integrated datasets remain accurate and up to date.
3. Interoperability and Standardization
Healthcare organizations are increasingly adopting healthcare data integration standards like HL7 and FHIR to improve system interoperability. Standardized data exchange supports smoother collaboration between providers, payers, and third-party applications, which ultimately streamlines data processing in healthcare and ensures consistent information flow.
4. Blockchain for Data Security
Blockchain offers a decentralized, tamper-proof method for securing sensitive medical records. By ensuring transparency and traceability, it strengthens compliance and builds patient trust in health data integration systems.
5. Internet of Things (IoT) and Real-Time Monitoring
With the rise of connected devices and wearables, real-time healthcare data integration is becoming essential. IoT-driven monitoring enables continuous patient tracking, timely interventions, and improved chronic disease management.
FAQs
Why is healthcare data integration important?
Healthcare data integration is important because it unifies fragmented patient information, enabling better clinical decisions, improved care coordination, and enhanced operational efficiency across healthcare systems.
What are the common challenges in healthcare data integration?
The biggest challenges include lack of interoperability, inconsistent data quality, privacy risks, high costs, and resistance to organizational change.
How do healthcare organizations integrate EHR and legacy systems?
Healthcare organizations use APIs, middleware, and healthcare data integration platforms to connect modern EHRs with legacy systems, ensuring smooth data flow and compatibility.
What role does data integration play in patient care?
Data integration gives providers a complete patient view, reducing errors, improving diagnostic accuracy, and supporting personalized treatment plans.
How does healthcare data integration support analytics and AI?
By combining clinical, operational, and patient-generated data, integration enables advanced analytics and AI models that predict risks, personalize care, and improve population health management.
How can healthcare organizations ensure data security and compliance?
They ensure compliance by following healthcare data integration standards, using encryption, role-based access, and adhering to HIPAA and GDPR frameworks.
What are the benefits of cloud-based healthcare data integration?
Cloud solutions offer scalability, cost-efficiency, real-time access, and interoperability, making them a preferred choice for modern healthcare systems.
How long does it take to implement healthcare data integration?
Implementation can take anywhere from a few months to over a year, depending on system complexity, data volume, and organizational readiness.
How do I choose the right healthcare data integration solution?
Organizations should assess interoperability features, compliance, scalability, and vendor expertise when selecting the right healthcare data integration platform.
Conclusion
Healthcare data integration is the foundation of modern, connected care breaking silos, enhancing decision-making, and enabling real-time insights that improve patient outcomes and reduce costs. As healthcare systems adopt cloud, AI, and IoT-driven solutions, robust integration becomes non-negotiable.
With proven expertise in EHR integration, secure architectures, and advanced analytics, Folio3 Data Services empowers healthcare providers to unlock the full potential of their data.
Partner with Folio3 to build scalable, compliant, and future-ready integration solutions!